Educating and advocating for quality, affordable, Universal Health Care in Oregon
Join the effort to bring Universal Health Care to Oregon
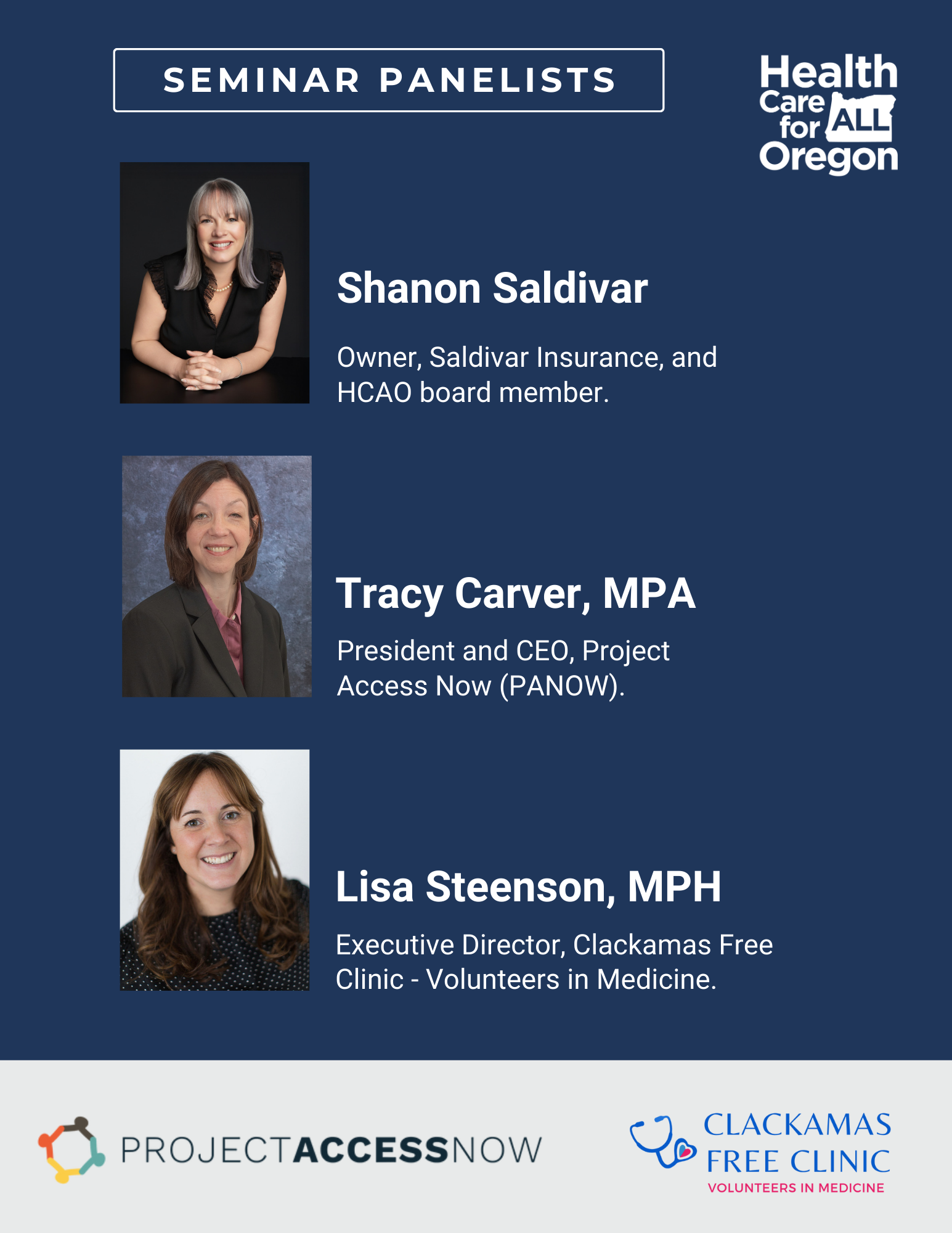
Medicaid and Marketplace Webinar: Bridging the Gap
Wednesday January 14th, 6:00 PM
Join us for this discussion on upcoming changes to American health insurance. We will start with an overview of Medicaid and Marketplace changes, with a focus on the impacts of HR1. Additionally, Project Access Now and Clackamas Free Clinic will discuss how they are working overtime to meet the need of the moment.
Sign this month’s testimony to the Universal Health Plan Governance Board
This month we are focusing our testimony on encouraging the Governance Board to increase their public engagement options.
Read our open letter to the Board, and share with your friends, and family. The deadline to sign is Sunday, January 11th at 7:00pm.
We are asking for UHPGB meetings outside of working hours so working class people can attend, recommending a meeting place outside of Salem, encouraging their main contractor to have dedicated focus group sessions for workers and unions, and to prioritize the health care consumers focus group.
HCAO in the News:
Washington County Chapter Chair Rebecca Hirsch was recently featured on Portland’s KOIN 6 morning program, Everyday Northwest. We’re so grateful for Rebecca’s description of what’s been happening in Oregon, and what’s at stake.
Watch the full interview for a great overview of our place in healthcare history, and the path ahead.

Events
There are community events every month furthering the work towards universal health care in Oregon!
The State of Oregon’s
Universal Health Plan Governance Board and Committees meet regularly.
They are developing our state’s universal health plan, due September 2026.
For the most updated meeting times and dates please click on the calendar below.
Follow the Board's and Committees' progress, and share your thoughts and feedback.
Register to attend any of their public meetings.
Learn About Universal Health Care
A simplified, equitable, affordable health care system that works for every Oregonian is in our future. Learn how and stay updated with the latest developments in Oregon's path to universal health care..
Get Involved
Sign up, volunteer, become a contributor, or take action today. Be part of the change!
Our Organization
HCAO is a statewide organization of 40,000 members and supporters.
Find out about our mission, methods, and the results of our years of education and advocacy.